First-generation DBM putties contain a filler, such as glycerol or reverse phase medium (RPM), solely to improve handling characteristics of the graft. The proportion of bone content in first-generation DBM putties can be as low as 17% by weight.1
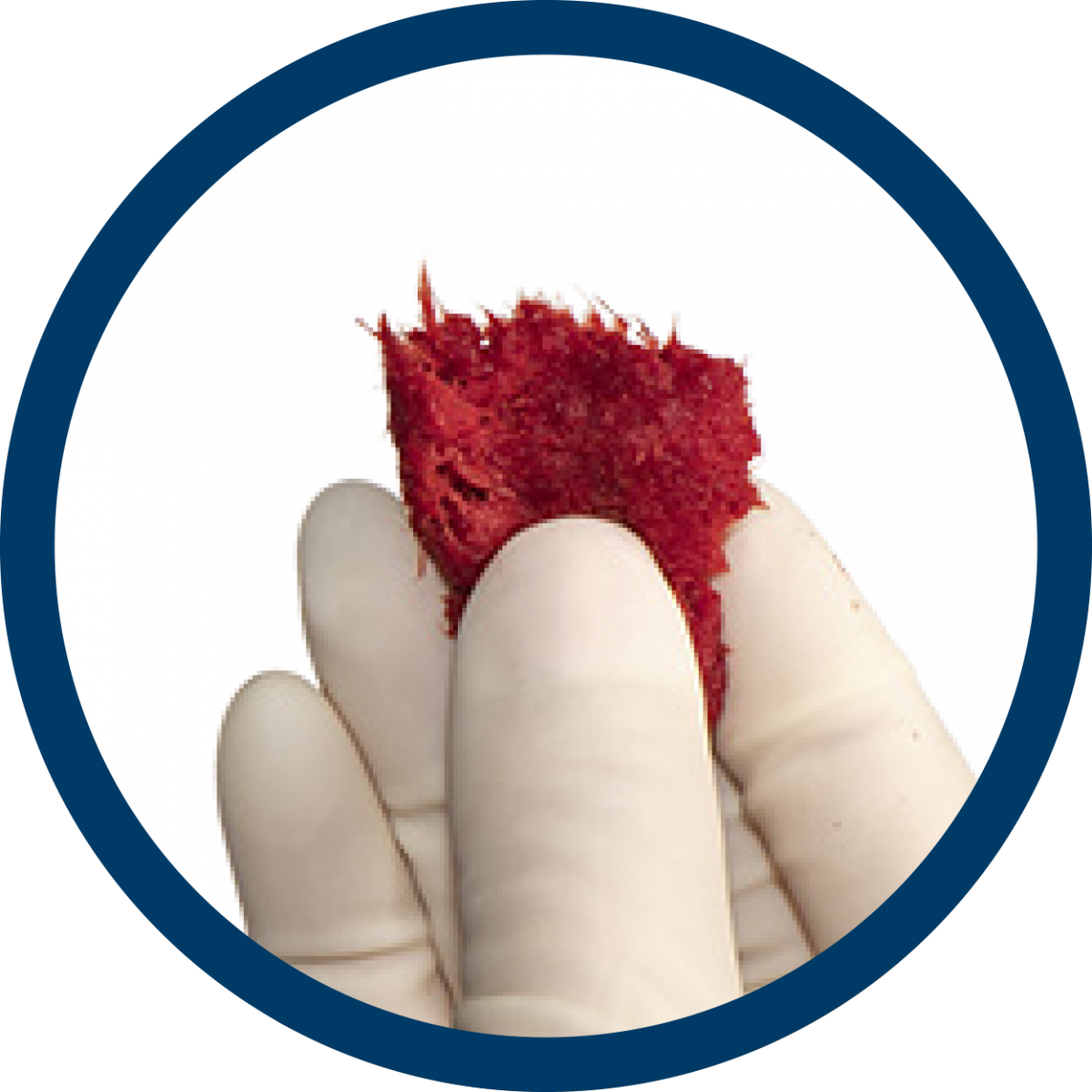
With PliaFX Prime, there is no compromise. The cortical bone fibers become moldable upon rehydration without the use of a filler that could dilute the osteoinductive potential of the graft.
100% bone provides undiluted value
When selecting a demineralized bone graft, consider how much of your investment goes towards bone, instead of the filler that does not participate in healing.3,4
Fillers can affect performance of demineralized bone
100% bone grows more bone than DBMs containing a filler, as demonstrated in literature.3,4
-
No dilution of osteoinductive potential.
-
Carrier can negatively impact the release of growth factors and their ability to promote new bone formation. 5
-
Carrier can negatively impact the functionality of native cells.6
-
Carrier can resorb quickly after implantation7,8 which creates potential for incomplete void fill.
-
ALP is a common marker of bone formation.

Alkaline phosphatase (ALP) is a marker of the early stages of new bone formation.
On average, PliaFX Prime exhibited 6.8x more ALP activity than DBM with a glycerol carrier
The importance of tissue processing
When comparing grafts from different tissue processors, both bone content and processing methods can affect the performance of the graft. For example, if a 100% bone graft has been processed in a way that damages or removes the components that contribute to bone formation, the performance of the graft could be adversely affected. LifeNet Health has nearly 40 years of experience with demineralized bone grafts, and utilizing validated and controlled processing methods to ensure implant quality and safety.
Kay, JF, Vaughan LM. Proportional osteoinduction of demineralized bone matrix graft materials. February 2004: AW-0204.1.
2.Shehadi JA, Elzein M. Review of commercially available demineralized bone matrix products for spinal fusions: A selection paradigm. Surgical Neurology International. 2017; 8: 203.
3.Boyan BD, Ranly DM, McMillan J, et al. Osteoinductive Ability of Human Allograft Formulations. J Periodontol. September 2006.
4.Data on file LifeNet Health TR-0446
5.Han B, Tang B, Nimni ME. Quantitative and sensitive in vitro assay for osteoinductive activity of demineralized bone matrix. J Orthop Res. 2003;21(4):648-654.
6.Murphy MB, Suzuki RK, Sand TT, et al. Short term culture of mesenchymal stem cells with commercial osteoconductive carriers provides unique insights into biocompatibility. J Clin. Med. 2013; 2,49-66; doi:10.3390/jcm2030049
7.Wang JC, Kanim LEA, Nagakawa S, et al. Dose-Dependent Toxicity of a Commercially Available Demineralized Bone Matrix Material. Spine. 2001;26(13):1429-1436.
Bostrum MPG, Yang X, Kennan M, et al. An Unexpected Outcome During Testing of Commercially Available Demineralized Bone Graft Materials. Spine. 2001;26(13):1425-1428.